Of the 1.2 million Americans living with HIV infection, 60% are not retained in medical care, 63% are not taking antiretroviral therapy (ART), and only 30% have undetectable viral loads, the ultimate goal of HIV treatment. African American/Black and Latino individuals are over-represented among those poorly engaged along this “HIV continuum of care.” Many barriers to ART and HIV medical care have been identified, ranging from factors that directly impact individuals (such as fear of side effects, medical distrust, and substance use problems), to factors that impact people indirectly through societal and environmental influences (such as insufficient social support or poor access to substance use treatment, mental health services, and HIV primary care). Typically, vulnerable persons living with HIV/AIDS (PLHA) face multiple barriers to ART and HIV care simultaneously, and barriers combine and interact with each other to reduce motivation, interfere with behavioral skills, and impede access to ART and HIV medical care, resulting in adverse health outcomes for PLHA, higher health care costs, and a higher probability of transmitting HIV to others.
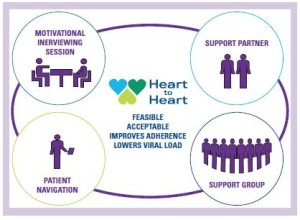 The Heart to Heart intervention is different than other interventions to address HIV care continuum problems because it is designed for PLHA who have delayed, declined, or discontinued ART. (There are many efficacious adherence programs but they are designed for those who are taking or will take ART.) Thus Heart to Heart is a “pre-adherence program.” Further, the problems of low uptake of ART and poor engagement in HIV care are related: Those who have declined ART may also avoid HIV care, because they do not wish to discuss or feel pressured to take ART, or because they do not see the need for HIV care if not on ART, and those not well engaged in HIV care rarely gain access to ART. Thus the Heart to Heart intervention also attends to poor engagement in HIV care. The Heart to Heart intervention has four main components—motivational interviewing sessions, involvement of support partners, focused support groups co-led by a “successful” peer on ART and engaged in HIV care, and patient navigation to link participants to HIV care and other needed supports and services—culturally targeted to the barriers and concerns most relevant to African American/Black and Latino PLHA.
The Heart to Heart intervention is different than other interventions to address HIV care continuum problems because it is designed for PLHA who have delayed, declined, or discontinued ART. (There are many efficacious adherence programs but they are designed for those who are taking or will take ART.) Thus Heart to Heart is a “pre-adherence program.” Further, the problems of low uptake of ART and poor engagement in HIV care are related: Those who have declined ART may also avoid HIV care, because they do not wish to discuss or feel pressured to take ART, or because they do not see the need for HIV care if not on ART, and those not well engaged in HIV care rarely gain access to ART. Thus the Heart to Heart intervention also attends to poor engagement in HIV care. The Heart to Heart intervention has four main components—motivational interviewing sessions, involvement of support partners, focused support groups co-led by a “successful” peer on ART and engaged in HIV care, and patient navigation to link participants to HIV care and other needed supports and services—culturally targeted to the barriers and concerns most relevant to African American/Black and Latino PLHA.
Heart to Heart was tested in a pilot randomized controlled trial. Ninety five participants were recruited mainly through community based organizations and peers. All participants were 18 years or older, had been HIV+ for at least 6 months, last CD4 count ≤500 cells/mm3, identified as African-American/Black or Latino/Hispanic, and had either never taken or had stopped taking ART.
- Overall, the Heart to Heart intervention was found to be feasible, with over 90% participation in the motivational interviewing component, 85% participation in patient navigation, and nearly 60% participation in the support groups. The support partner component was not feasible, but participants indicated the critical need for the involvement of successful peers in the program.
- Further, qualitative research indicated that it was well regarded by participants, that is, highly acceptable.
- Good adherence, that is, taking ART 7 days a week, as measured by objective biological testing of hair samples, was more than twice as likely among those in the intervention arm (60% vs. 27%).
- Among those who initiated ART, 8 months after enrollment HIV viral load was more than one and a half times higher in the control arm, with the intervention reducing viral load by 35%.
- Rates of engagement in HIV care did not improve significantly.
This study points to a new culturally targeted, multi-component, behavioral intervention strategy to improve uptake of ART and reduce HIV viral load for vulnerable PLHA who have declined, delayed, or discontinued ART.
Gwadz M, Cleland CM, Applegate E, Belkin M, Gandhi M, Salomon N, Banfield A, Leonard N, Riedel M, Wolfe H, Pickens I, Bolger K, Bowens D, Perlman D, Mildvan D, and the Heart to Heart Collaborative Research Team (2015).
Behavioral intervention improves treatment outcomes among HIV-infected individuals who have delayed, declined, or discontinued antiretroviral therapy: A randomized controlled trial of a novel intervention
AIDS and Behavior, 19 (10), 1801-1807. doi: 10.1007/s10461-015-1054-6. PMCID: PMC4567451.
Or contact Marya Gwadz: mg2890@nyu.edu
The HTH study was supported by a grant by the National Institutes of Mental Health (R34MH093352) and by the Center for Drug Use and HIV Research (P30DA011041, NIDA).